The precise nature of proton therapy makes it an excellent treatment option for liver cancer including both primary and secondary liver cancers. Because the liver plays a vital role in filtering toxins and producing essential proteins, any disease affecting it can be particularly challenging. Many liver cancers develop in patients who already have chronic liver conditions like cirrhosis or hepatitis which can complicate treatment.
Types of Liver Cancer
There are two main categories of liver cancer:
Primary liver cancer originates in the liver itself. The most common type is hepatocellular carcinoma (HCC). Less common types include intrahepatic cholangiocarcinoma (bile duct cancer) and rare forms, like angiosarcoma.
Secondary liver cancer (metastases) occurs when cancer from another part of the body such as the colon, breast, or lung, spreads to the liver.
When Surgery Is Not an Option
Surgery to remove the tumor is often the preferred treatment but many patients are not candidates due to poor liver function from underlying disease, the tumor's size or location, or other health issues. Liver transplantation may be considered for select patients with early-stage cancer and severe underlying liver disease, but donor organ availability limits this option.
When surgery is not possible or insufficient, proton therapy provides a powerful, non-invasive alternative that can be used alone or with other treatments, like chemotherapy or immunotherapy.
The Difference Proton Therapy Can Make
Liver cancers were among the earliest cancers to be treated with proton radiotherapy.¹⁻³ This is because the liver is uniquely suited to benefit from the characteristics of protons.
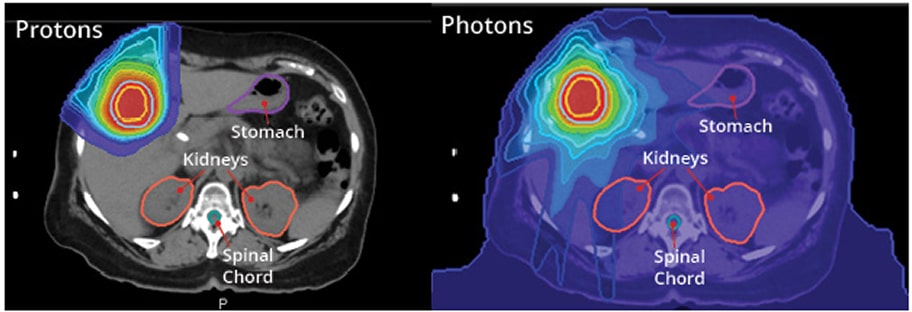
Traditional radiation is often limited by the risk of harming the sensitive liver tissue and nearby organs like the stomach, intestines and kidneys. Proton therapy overcomes this challenge by delivering a powerful dose of radiation that stops precisely at the tumor, sparing surrounding healthy tissue. This precision is critical for patients with preexisting liver disease.
This ability to protect healthy tissue allows physicians to use higher, more effective radiation doses to destroy the tumor, reducing the risk of side effects and helping to preserve vital liver function.
Clinically Proven
Thousands of patients worldwide have been treated with advanced radiation therapy for liver cancer with multiple clinical trials demonstrating significant benefits, including but not limited to:
- Significant improvement in overall survival and reduced risk of radiation induced liver decompensation with proton therapy compared to traditional photon radiation for unresectable hepatocellular carcinoma.4
- Improved survival when radiation is used with targeted therapy over targeted therapy alone in patients with advanced liver cancer.⁵
- Superior tumor control with less severe complications compared to other local modality.6-7
- Clinical studies consistently show that SBRT and proton therapy achieve local tumor control rates of 90%.8-9
Treatment Applications for Proton Therapy
Proton therapy is a flexible tool that can be used in several ways:
Primary Treatment: For patients who are not candidates for surgery.
Bridge Therapy: To control cancer for patients awaiting a liver transplant.
Salvage Therapy: To treat tumors that remain or recur after other treatments have failed. The precision of protons often allows for re-treating an area if cancer returns.
Combination Therapy: Used with systemic treatments to improve overall outcomes.
Physicians at the University of Florida Health Proton Therapy Institute are using the most advanced proton therapy techniques to treat both primary and secondary liver cancers offering hope to patients with even the most complex cases.
Information for Treatment Evaluation
To evaluate if you are a candidate for proton therapy, you may be asked to provide:
- A complete medical history, including dates of biopsies, surgeries and other treatments
- Recent liver function test results
- All imaging studies (CT, MRI, PET scans) with reports and images on a compact disk
- Pathology reports from any biopsies
- Hepatitis B and C status
- Alpha-fetoprotein (AFP) levels
- Information on underlying liver disease or cirrhosis
If you are interested in liver cancer treatment with proton therapy and would like to know if you are eligible, contact the UF Health Proton Therapy Institute today.
References
1 B1. Kawashima M, Furuse J, Nishio T, et al. Phase II study of radiotherapy employing proton beam for hepatocellular carcinoma. J Clin Oncol. 2005;23(9):1839-1846.
2 Mizumoto M, Oshiro Y, Okumura T, et al. Proton beam therapy for hepatocellular carcinoma: A review of the University of Tsukuba experience. Int J Part Ther. 2016;2(4):570-578.
3 Nakayama H, Sugahara S, Tokita M, et al. Proton beam therapy for hepatocellular carcinoma. Cancer. 2009;115(23):5499-5506.
4 Sanford NN, Pursley J, Noe B, et al. Protons versus photons for unresectable hepatocellular carcinoma: Liver decompensation and overall survival. Int J Radiat Oncol Biol Phys. 2019;105(1):64-72.
5 Dawson LA, et al. Randomized trial of stereotactic body radiotherapy for hepatocellular carcinoma: RTOG 1112. J Clin Oncol. 2023.
6 Romero AM, et al. Stereotactic body radiation therapy versus drug-eluting bead transarterial chemoembolization for hepatocellular carcinoma: TRENDY trial. Int J Radiat Oncol Biol Phys. 2023;116(4):797-806.
7 Bush DA, et al. Proton beam radiotherapy versus transarterial chemoembolization for hepatocellular carcinoma: Results of a randomized trial. Cancer. 2023;129(20):3554-3563.
8 Bae SH, et al. Stereotactic body radiotherapy for hepatocellular carcinoma: meta-analysis and international stereotactic radiosurgery society practice guidelines. Int J Radiat Oncol Biol Phys. 2023;117(1):123-139.
9 Coffman AR, et al. Proton stereotactic body radiation therapy for liver metastases-results of 5-year experience for 81 hepatic lesions. J Gastrointest Oncol. 2021 Aug;12(4):1753-1760. doi: 10.21037/jgo-20-424. PMID: 34532125; PMCID: PMC8421917.
Cancer Treatment Specialist(s)